Updated terminology for gamete and embryo donors: directed (identified) to replace ‘‘known’’ and nonidentified to replace ‘‘anonymous’’: a committee opinion (2022)
Gamete and embryo donation have historically been characterized as known or anonymous. The terminology reflected what was true at one time; donors and recipients either knew one another or did not at the time of the donation. For those who were unknown to each other at the time of the donation, the expectation was that this anonymity would continue indefinitely. The identity of anonymous donors was protected by both clinical protocols and, to varying degrees, legislation intended to address legal parentage of recipients and non-parentage of donors.
Social media, changing mores, and more recently significantly broader access to direct-to-consumer deoxyribonucleic acid (DNA) testing (DTC DNA) have all contributed to a new reality that expectations of donor anonymity can no longer be assured. It is estimated that at the present time, tens of millions of Americans have their genetic information stored in privately owned and largely unregulated databases (1).
Other modalities such as facial recognition have also recently become refined and more accurate (2). These technologies have introduced a means by which donor-conceived offspring and those to whom they have genetic ties may identify, locate, and contact one another. It should be noted that individuals who donated gametes or embryos, or who are donor conceived, may be traceable even if they never enroll in any DNA testing program themselves. This may occur if others with genetic ties to them participate in DTC DNA programs that allow for the identification of those to whom they are genetically linked (3). The era of perpetual donor anonymity has ended. This loss of anonymity has the potential to affect both current and past donations, including donors, recipients, donor-conceived offspring, and those who are genetically linked to them. While donor identity can still be withheld at the time of a donation, the discovery of genetic relationships leading to gamete and embryo donor identification may occur both outside the control of medical professionals and indefinitely into the future.
These emerging genetic and technological realities have changed the landscape of gamete and embryo donation, necessitating a concomitant change in the language used to describe these donations and in the counseling of those who participate in them.
As such, the American Society for Reproductive Medicine has changed the nomenclature of gamete and embryo donation. Donors who were previously described as known will now be referred to as directed (identified) donors, and those previously described as anonymous will be referred to as non- identified donors.
Example of unplanned identification (Figure 1): Family A: Use of donor gamete never disclosed to child. Family B: ‘‘Anonymous’’ gamete donation never disclosed by the donor. Children A and B: Independently send DNA to a DTC DNA Laboratory without parental knowledge. Each is notified about a 1/2 sibling. Difficult conversations ensue.
Social media, changing mores, and more recently significantly broader access to direct-to-consumer deoxyribonucleic acid (DNA) testing (DTC DNA) have all contributed to a new reality that expectations of donor anonymity can no longer be assured. It is estimated that at the present time, tens of millions of Americans have their genetic information stored in privately owned and largely unregulated databases (1).
Other modalities such as facial recognition have also recently become refined and more accurate (2). These technologies have introduced a means by which donor-conceived offspring and those to whom they have genetic ties may identify, locate, and contact one another. It should be noted that individuals who donated gametes or embryos, or who are donor conceived, may be traceable even if they never enroll in any DNA testing program themselves. This may occur if others with genetic ties to them participate in DTC DNA programs that allow for the identification of those to whom they are genetically linked (3). The era of perpetual donor anonymity has ended. This loss of anonymity has the potential to affect both current and past donations, including donors, recipients, donor-conceived offspring, and those who are genetically linked to them. While donor identity can still be withheld at the time of a donation, the discovery of genetic relationships leading to gamete and embryo donor identification may occur both outside the control of medical professionals and indefinitely into the future.
These emerging genetic and technological realities have changed the landscape of gamete and embryo donation, necessitating a concomitant change in the language used to describe these donations and in the counseling of those who participate in them.
As such, the American Society for Reproductive Medicine has changed the nomenclature of gamete and embryo donation. Donors who were previously described as known will now be referred to as directed (identified) donors, and those previously described as anonymous will be referred to as non- identified donors.
DIRECTED DONORS
The choice of the term directed (identified) donor, previously called known donor, was selected to align with the Food and Drug Administration (FDA) regulations (4). The gametes from a directed (identified) donor who is deemed ‘‘ineligible’’ based on FDA guidance for tissue donation may in some cases be used if both parties are aware of the theoretical infectious or genetic risks to the recipient(s) and offspring and consent to move forward with the donation (5). The categorization of an individual as a directed (identified) donor affords recipients the option of waiving some exclusion criteria when they value the benefits of the known donor (e.g., sister to sister egg donation) so strongly that they are willing to accept the presumably low risk of infectious disease transmission. The use of the term directed (identified) mirrors the FDA language that specifies exclusions and exceptions for gamete and embryo donation based on whether the parties are known to one another. The new terminology should assist physicians and administrators as they interpret and apply the FDA regulations to clinical practice.NONIDENTIFIED DONORS
The choice of the term nonidentified for those who were previously called anonymous donors acknowledges the intention of all involved in the donation process, including donors and recipients, as well as any medical, professional, or coordinating entities or professionals, not to share identifying information of the donor or recipient with one another. The intention at the time a nonidentified donation contract is entered into, or the donation undertaken, is that the identities of the donor, recipient, and any resulting offspring will remain unknown to one another to the extent permitted under law or to an explicit and limited degree, such as when a contract or consent document may allow for arranging contact between the donor-conceived offspring and the donor upon the offspring reaching a specific age, often the age of majority. These latter types of arrangements are sometimes referred to as open-identity arrangements, and the donors who agree to them are referred to as open-identity donors.Example of unplanned identification (Figure 1): Family A: Use of donor gamete never disclosed to child. Family B: ‘‘Anonymous’’ gamete donation never disclosed by the donor. Children A and B: Independently send DNA to a DTC DNA Laboratory without parental knowledge. Each is notified about a 1/2 sibling. Difficult conversations ensue.
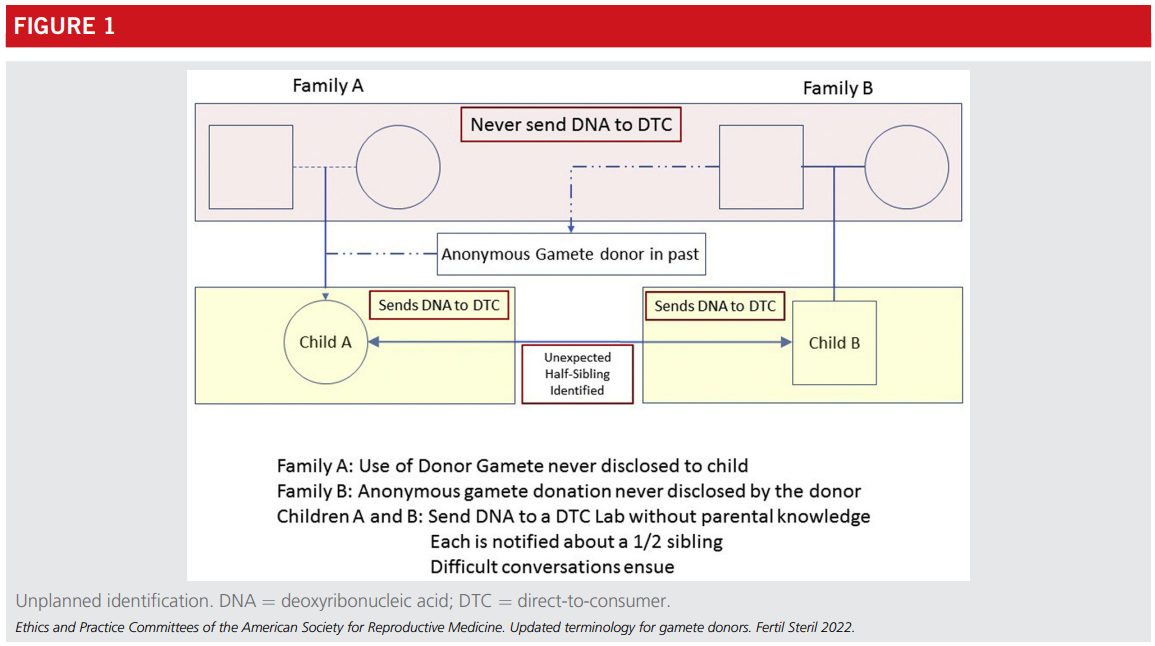
This scenario applies equally to egg, sperm, and embryo donation. Furthermore, it need not be the donor-conceived offspring who participate; it could be other genetically related individuals. Finally, in cases of directed gamete donation, where the donor and recipient are known to one another, the parties involved will want to consider who are the other genetic relatives that should be made privy to the information, as they may inadvertently find out about the donation at some future date if they participate in genetic testing.
The impact that this will have on those being discovered and whether this current reality will change the willingness of individuals to serve as gamete or embryo donors remain to be seen. The collateral effects on genetically linked individuals much removed from the donation process are also unknown but will become clearer over time. Critical to the donation process is the informed consent of donors and recipients regarding the possibility that genetically linked individuals may identify one another, both intentionally and otherwise, at any future date.
Physicians and those who arrange gamete and embryo donation should provide maximum transparency regarding the limits of anonymity to all known stakeholders at the time of the donation, beginning with the change in nomenclature when referring to directed (identified) and nonidentified gamete and embryo donors.
Acknowledgments: This report was developed under the direction of the Practice and Ethics Committees of the American Society for Reproductive Medicine (ASRM) as a service to its members and other practicing clinicians. Although this document reflects appropriate management of a problem encountered in the practice of reproductive medicine, it is not intended to be the only approved standard of practice or dictate an exclusive course of treatment. Other plans of management may be appropriate, taking into account the needs of the individual patient, available resources, and institutional or clinical practice limitations. The Practice and Ethics Committees and the Board of Directors of the American Society for Reproductive Medicine have approved this report.
This document was reviewed by the ASRM members, and their input was considered in the preparation of the final document. The following members of the ASRM Practice and Ethics Committees participated in the development of this document: Alan Penzias, MD; Kristin Bendikson, MD; Marcelle I. Cedars, MD; Tommaso Falcone, MD; Karl Hansen, MD, PhD; Micah Hill, DO; Sangita Jindal, PhD; Suleena Kalra, MD, MSCE; Jennifer Mersereau, MD; Catherine Racowsky, PhD; Richard Reindollar, MD; Chevis N Shannon, DrPH, MPH, MBA; Anne Steiner, MD, MPH; Cigdem Tanrikut, MD; Michael Thomas, MD; Belinda Yauger, MD; Sigal Klipstein, MD; Deborah Anderson; Kavita Shah Arora, MD, MBE; Tolulope Bakare, MD; Katherine Cameron, MD; Susan Crockin, JD; Ruth Farrell, MD; Catherine Hammack-Aviran, MA, JD; Mandy Katz-Jaffe, PhD; Jennifer Kawwass, MD; Ed- ward Martinez, MD; Joshua Morris, MD; Robert Rebar, MD; Eli Reshef, MD; Chevis N Shannon, DrPH, MPH, MBA; Hugh Taylor, MD; Sean Tipton, MA; and Julianne Zweifel, PhD. All Committee members disclosed commercial and financial relationships with manufacturers or distributors of goods or services used to treat patients. The members of the Committees who were found to have conflicts of interest based on the relationships disclosed did not participate in the discussion or development of this document.
CONCLUSION
In conclusion, given a multitude of global social media platforms, increasingly accessible and used DTC DNA services, and facial recognition technology, true anonymity between donors and recipients can no longer be guaranteed. All parties involved in gamete and embryo donation should be aware that identities may be discovered by the resulting offspring and other genetically linked individuals at any future time. This holds for both directed (identified) and nonidentified do- nations. Complicating matters is the fact that past donors, whether they donated with the intention of anonymity or not, are now potentially discoverable at any future date. The extent to which such revelations will occur is unknown. A 2019 estimate suggested that approximately 8% of the US population had already sent DNA to a DTC DNA vendor with speculation that the number could more than triple over the next several years, thus greatly expanding the population of people who can identify one another based on their genetic links (6). A related, but somewhat different, scenario is the active pursuit of connection among offspring who know they were conceived from donor gametes or embryos (7).The impact that this will have on those being discovered and whether this current reality will change the willingness of individuals to serve as gamete or embryo donors remain to be seen. The collateral effects on genetically linked individuals much removed from the donation process are also unknown but will become clearer over time. Critical to the donation process is the informed consent of donors and recipients regarding the possibility that genetically linked individuals may identify one another, both intentionally and otherwise, at any future date.
Physicians and those who arrange gamete and embryo donation should provide maximum transparency regarding the limits of anonymity to all known stakeholders at the time of the donation, beginning with the change in nomenclature when referring to directed (identified) and nonidentified gamete and embryo donors.
Acknowledgments: This report was developed under the direction of the Practice and Ethics Committees of the American Society for Reproductive Medicine (ASRM) as a service to its members and other practicing clinicians. Although this document reflects appropriate management of a problem encountered in the practice of reproductive medicine, it is not intended to be the only approved standard of practice or dictate an exclusive course of treatment. Other plans of management may be appropriate, taking into account the needs of the individual patient, available resources, and institutional or clinical practice limitations. The Practice and Ethics Committees and the Board of Directors of the American Society for Reproductive Medicine have approved this report.
This document was reviewed by the ASRM members, and their input was considered in the preparation of the final document. The following members of the ASRM Practice and Ethics Committees participated in the development of this document: Alan Penzias, MD; Kristin Bendikson, MD; Marcelle I. Cedars, MD; Tommaso Falcone, MD; Karl Hansen, MD, PhD; Micah Hill, DO; Sangita Jindal, PhD; Suleena Kalra, MD, MSCE; Jennifer Mersereau, MD; Catherine Racowsky, PhD; Richard Reindollar, MD; Chevis N Shannon, DrPH, MPH, MBA; Anne Steiner, MD, MPH; Cigdem Tanrikut, MD; Michael Thomas, MD; Belinda Yauger, MD; Sigal Klipstein, MD; Deborah Anderson; Kavita Shah Arora, MD, MBE; Tolulope Bakare, MD; Katherine Cameron, MD; Susan Crockin, JD; Ruth Farrell, MD; Catherine Hammack-Aviran, MA, JD; Mandy Katz-Jaffe, PhD; Jennifer Kawwass, MD; Ed- ward Martinez, MD; Joshua Morris, MD; Robert Rebar, MD; Eli Reshef, MD; Chevis N Shannon, DrPH, MPH, MBA; Hugh Taylor, MD; Sean Tipton, MA; and Julianne Zweifel, PhD. All Committee members disclosed commercial and financial relationships with manufacturers or distributors of goods or services used to treat patients. The members of the Committees who were found to have conflicts of interest based on the relationships disclosed did not participate in the discussion or development of this document.
REFERENCES
- Regalado A. 2017 was the year consumer DNA testing blew up. Available at: https://www.technologyreview.com/2018/02/12/145676/2017-was-the-year- consumer-dna-testing-blew-up/. Accessed March 23, 2022.
- Harwell D. This facial recognition website can turn anyone into a cop—or a stalker. Available at: https://www.washingtonpost.com/technology/2021/ 05/14/pimeyes-facial-recognition-search-secrecy. Accessed March 23, 2022.
- 23andMe Customer Care. What unexpected things might I learn from 23andMe?. Available at: https://customercare.23andme.com/hc/en-us/ articles/202907980. Accessed March 23, 2022.
- US Food and Drug Administration. Eligibility determination for donors of human cells, tissues, and cellular and tissue-based products: guidance for industry. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance- documents/eligibility-determination-donors-human-cells-tissues-and- cellular-and-tissue-based-products. Accessed March 23, 2022.
- Practice Committee of the American Society for Reproductive Medicine, Practice Committee for the Society for Assisted Reproductive Technology. Guidance regarding gamete and embryo donation. Fertil Steril 2021;115:1395–410.
- Regalado A. More than 26 million people have taken an at-home ancestry test. Available at: https://www.technologyreview.com/2019/02/11/103446/ more-than-26-million-people-have-taken-an-at-home-ancestry-test. Ac- cessed March 23, 2022.
- Dominus S. Sperm donors can’t stay secret any more. Here’s what that means. Available at: https://www.nytimes.com/2019/06/26/magazine/sperm-donor- questions.html. Accessed March 23, 2022.
Ethics Opinions
Ethics Committee Reports are drafted by the members of the ASRM Ethics Committee on the tough ethical dilemmas of reproductive medicine.

Family members as gamete donors or gestational carriers: an Ethics Committee opinion (2024)
The use of adult intrafamilial gamete donors and gestational surrogates is ethically acceptable when all participants are fully informed and counseled.
Financial ‘‘risk-sharing’’ or refund programs in assisted reproduction: an Ethics Committee opinion (2023)
Financial ‘‘risk-sharing’’ fee structures in programs charge patients a higher initial fee but provide reduced fees for subsequent cycles.
Planned oocyte cryopreservation to preserve future reproductive potential: an Ethics Committee opinion (2023)
Planned oocyte cryopreservation is an ethically permissible procedure that may help individuals avoid future infertility.
Ethical obligations in fertility treatment when intimate partners withhold information from each other: an Ethics Committee opinion (2024)
Clinicians should encourage disclosure between intimate partners but should maintain confidentiality where there is no harm to the partner and/or offspring.Practice Documents
ASRM Practice Documents have been developed to assist physicians with clinical decisions regarding the care of their patients.
Current evaluation of amenorrhea: a committee opinion (2024)
Amenorrhea is the absence or abnormal cessation of the menses.
Inclusive language and environment to welcome lesbian, gay, bisexual, transgender, queer, questioning, intersex, and asexual+ patients (2024)
Creating an inclusive clinical environment to serve lesbian, gay, bisexual, transgender, queer, questioning, intersex, and asexual+ patients is vital.
Subclinical hypothyroidism in the infertile female population: a guideline (2024)
This guideline reviews the risks and benefits of treating subclinical hypothyroidism in female patients with a history of infertility and miscarriage.
Tobacco or marijuana use and infertility: a committee opinion (2023)
In the United States, approximately 21% of adults report some form of tobacco use, although 18% report marijuana use.Topic Resources
View more on the topic of egg donation
Topic Resources
View more on the topic of embryo donation
Topic Resources
View more on the topic of sperm donation